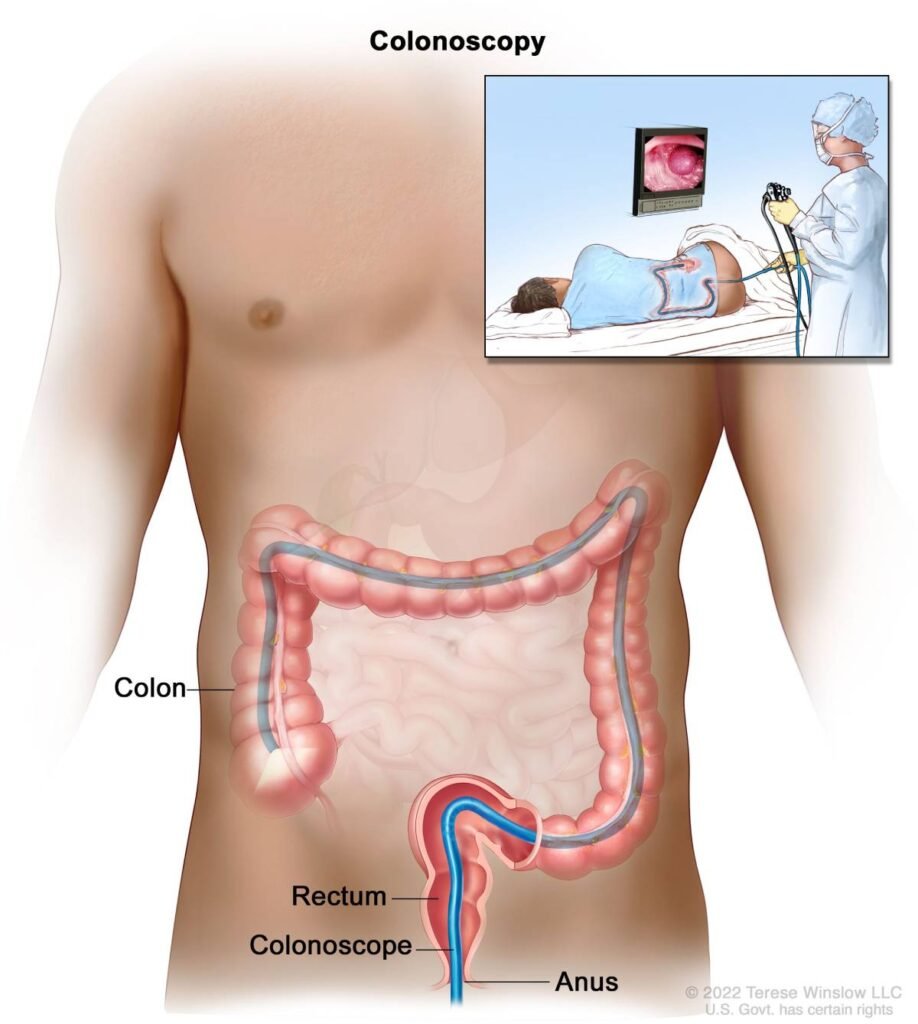
A colonoscopy is a medical procedure used to examine the inside of the large intestine (colon and rectum). It is the most effective method for detecting colon cancer, polyps, inflammation, and bleeding.
.
Why It’s Done (Indications)
✅ Screening & Prevention
- Colorectal cancer screening (usually starting at age 45)
- Check for polyps (precancerous growths)
✅ Diagnosis
- Investigate symptoms such as:
- Blood in stool
- Chronic diarrhea or constipation
- Abdominal pain or cramping
- Unexplained weight loss
- Iron-deficiency anemia
✅ Monitoring
- Surveillance for patients with:
- A history of polyps
- Colorectal cancer
- Inflammatory bowel disease (Crohn’s or ulcerative colitis)
🔹 How to Prepare
Bowel Preparation (“Prep”) is crucial for clear visibility during the exam:
- Diet changes (usually 1–3 days before):
- Switch to clear liquids (broth, water, clear juice)
- Avoid solid food and red/purple liquids
- Laxatives or prep solutions:
- Taken the night before and sometimes the morning of the procedure
- Helps completely empty the colon
- Stop certain medications:
- Your doctor may advise you to pause blood thinners, iron supplements, or diabetes meds
🔹 What Happens During a Colonoscopy
- The procedure is done in a hospital or clinic.
- You’ll receive sedation or anesthesia (you’ll be asleep or very relaxed).
- A long, flexible tube (colonoscope) with a camera is inserted through the anus and advanced through the rectum and colon.
- The doctor examines the colon lining on a video screen.
- Biopsie
Test | Description | Invasiveness | Frequency |
Colonoscopy | Direct visual exam of colon | Invasive | Every 10 yrs (normal results) |
FIT (Fecal Test) | Detects hidden blood in stool | Non-invasive | Yearly |
Cologuard (DNA test) | Detects abnormal DNA and blood in stool | Non-invasive | Every 3 yrs |
Sigmoidoscopy | Examines lower part of colon only | Invasive | Every 5 yrs |
- s or polyp removal can be done during the procedure if needed.
🕒 Duration: 20–45 minutes (you’ll stay longer for sedation recovery)
🔹 After the Procedure
- You’ll rest for 30–60 minutes until the sedation wears off.
- You cannot drive home – arrange for someone to accompany you.
- Mild bloating, gas, or cramping is normal and temporary.
- You can usually eat normally after recovery.
🔹 Risks and Complications (Rare)
- Bleeding (especially if a polyp is removed)
- Perforation (tear in the colon wall)
- Adverse reaction to sedation
- Infection (very rare)
🔹 Colonoscopy vs. Other Tests
🔹 When to Get Screened
- Starting at age 45 for average-risk individuals
- Earlier or more often if:
- Family history of colorectal cancer/polyps
- Personal history of IBD
- Genetic conditions (e.g., Lynch syndrome, FAP)
❗️Contact Your Doctor If After the Procedure You Have:
- Severe abdominal pain
- Fever or chills
- Heavy rectal bleeding
- Dizziness or weakness



